‘The virus is always evolving’
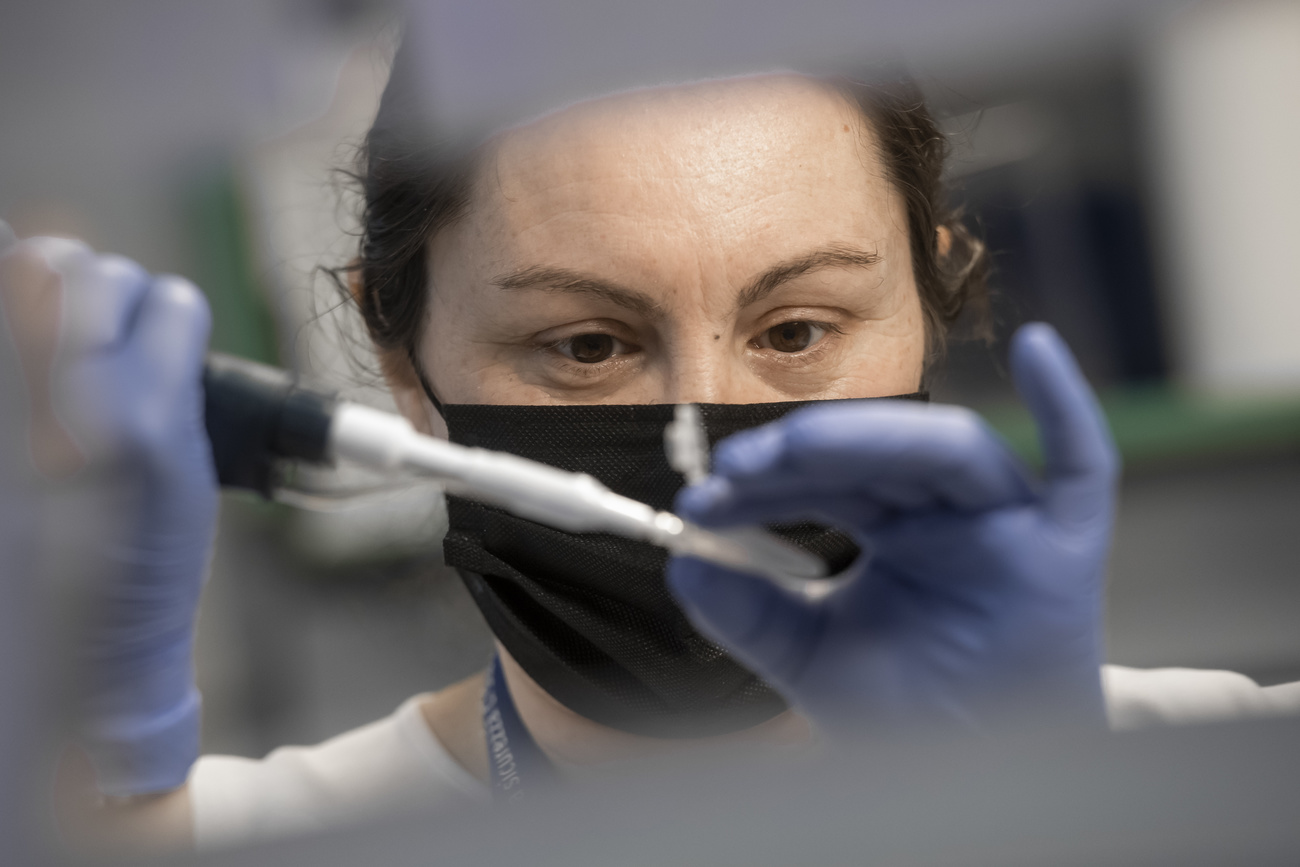
Should we be afraid of virus variants? Will vaccines be effective against these new virus forms? Emma Hodcroft, a genomic epidemiologist at the Institute of Social and Preventive Medicine in Bern, discusses mutations and how vaccines are developed.
Covid-19 variants worry scientists and governments – with good reason. According to British-American epidemiologist Emma Hodcroft, it is essential to keep infections low and contain the spread of variants. Though mutations are a normal part of virus life, in rare cases, they can generate much more dangerous variants.
SWI swissinfo.ch: What do we know about these mutations?
Emma Hodcroft: There are three main variants that are attracting scientists’ attention at the moment. A fourth variant is making headlines, but scientists don’t know how much of a concern it is yet. The variants are mainly found in the United Kingdom and South Africa, and two others have appeared in Brazil. The one circulating in Britain is the first one that was discovered. From the data we have, it is spreading locally in most European countries. This variant is causing concern because it is more contagious and therefore more difficult to manage than, for example, the SARS-CoV-2 variants that were circulating this summer. Although there is no clear indication that it is more dangerous or lethal, the more people that get infected and get sick, the more the stress this is adding to the health care system. This is what we are seeing in the UK.
We have less information on the other variants. The variant in South Africa shares a common mutation with the UK one. It has an additional mutation that is of particular concern to scientists. The two variants circulating in Brazil also have this mutation. According to some studies, this variant is transmitted much faster, but we still do not have enough data to be certain. What is really alarming is that the additional mutation could make the virus capable of re-infecting people who have already contracted SARS-CoV-2. And this of course could also affect the effectiveness of vaccines. The good news is that that recent data released by Moderna suggests that the vaccine response to these mutations is still good enough to work.

SWI: Does this mean that mutations could affect the vaccines?
EH: Even if vaccines become less effective, it is unlikely that they would stop working altogether. The issue is that efficacy could drop from 95% to 85-90%.
Experience with other pathogens has shown that the immune response you get from vaccines is better than the naturally generated response. Vaccines are better at teaching our bodies how to defend themselves. If this is true with SARS-CoV-2, then it could be that this mutation doesn’t affect vaccines at all – or only to a small degree. From the recent Moderna data, it seems this is the case.
SWI: Do these mutations worry you?
EH: From a scientific perspective, the evolution of the virus is completely normal and there is nothing surprising about it. The issue is that every time the virus replicates, there is a chance that an error will occur, and that this will generate a mutation. The longer we play this game, the higher the odds are that the next mutation will be one we don’t want to see.
We will never be able to rule out such as scenario, or prevent it entirely, unless we wipe the virus off the face of the earth. However, we can certainly reduce the possibility by making sure that the virus has less access to unusual situations or people who don’t have good immune systems. That is where the virus finds a favorable playing field. We shouldn’t underestimate the lesson we’ve learned in recent months: even if something is unlikely, it doesn’t mean it won’t happen. The longer we give the virus space, the more risk we take that the next mutation will be bad news. It’s important to remember that the virus is always evolving, and although the vast majority of these mutations are harmless, it’s in our best interest to keep the number of cases as low as possible.
SWI: In the media these variants are referred to as British or South African. Is this where they came from? How do scientists study the origins of mutations?
EH: It is really hard not to use these geographical names because they have entered everyday and media use and it is often the clearest way to identify variants. For our part, we avoid using them as much as possible because they can severely damage the reputation of these countries. In addition, they are not entirely appropriate because it is difficult to know for sure where the mutations originated.
What we can say with some degree of certainty is that the variant present in the UK, for example, may not have originated there but grew there. The high number of sequences found and the spread across the UK seem to suggest that it spread there rather than elsewhere in Europe.
For Brazil and South Africa, it is more difficult to determine the origin of the mutations. These are not isolated countries like Great Britain, but they border other countries. South Africa does quite well with sequencing, but many of its neighbors are unable to. As such, we do not know if the mutation happened in another southern African state and was then detected in South Africa. The situation is even more complex in South America because Brazil and its neighbours don’t have good sequencing capabilities.

SWI: Is it important from a scientific point of view to know the exact origin of a mutation?
EH: Yes, it is important to know which environments could favor certain mutations and to act to stop their spread. For example, in an environment where there are many infections, the virus gains an advantage from the mechanism of reinfection. That advantage is minimal where cases are low. From this perspective, it is relevant to understand how different environments can stimulate the production of these variants.
SWI: Do you think cases of the so-called British variant could explode in Switzerland as they have in the UK? Are stricter measures necessary?
EH: The British variant is already circulating in Switzerland and we should prepare for the fact that the situation could get worse. That’s why to stop the trend, it’s very important to keep infections down. It is a strategy from which we can only benefit, because if we manage to contain it, then we can stop the spread. On the other hand, if we fail to contain it but still get cases down, we can spare our healthcare system from being overloaded – which means it will be able to respond if the situation gets worse. We don’t want to end up with a severely strained system and ambulance queues outside hospitals, as has been the case in the UK.
SWI: Has the fight against the virus become a race against time?
EH: I wouldn’t look at it from that point of view. It’s unlikely that we’re going to be able to vaccinate the population faster than the variant spreads. Rather, until the whole population can be vaccinated, we need to focus on keeping cases down through social distancing and hygiene.
SWI: Are the concerns against the vaccine justified?
EH: A lot of concerns have arisen about how quickly these vaccines have been developed. Many have heard that it normally takes five to ten years to get a vaccine on the market. First of all, it’s important to clarify that many of the vaccines approved had already been developed for other viruses, in some cases for other coronaviruses. We are not starting from scratch. Second, what lengthens the time to develop a vaccine is not the science, but the bureaucracy around it. A big part of a scientist’s job is finding funding, writing reports, and convincing enough volunteers to enroll in trials of new vaccines. All of this makes the process long and difficult. The coronavirus pandemic has eliminated many of these problems. Governments gave money and provided infrastructure very quickly and an incredible number of people wanted to test the vaccines. Science was not quicker; bureaucracy was. These vaccines were tested even more thoroughly than most because there were so many volunteers. This is a testament to where science can go when there is cooperation among all interest groups.
Another concern among the population is the long-term effects. Vaccines stay in the body long enough to teach the immune system how to fight a certain virus, and then they disappear. This is why they have very few side effects and are much less dangerous than the virus in a natural infection, because they are not infectious and therefore do not cause organ damage, as we have seen in the case of the coronavirus.
SWI: What lessons does this pandemic teach us for the future?
EH: It teaches us that we still know too little about viruses. Much research has focused on influenza viruses and HIV, but the importance of coronaviruses, and other viruses, has been underestimated. There are thousands of viruses out there and we don’t know when the next pandemic will come. I hope that what is happening now will help raise awareness of the importance of virus research.
Emma Hodcroft is a British-American genomic epidemiologist at the Institute of Social and Preventive Medicine at the University of Bern. During the Covid-19 pandemic, her work has focused on studying SARS-CoV-2 variants from the genetic sequences of the virus made available by scientists around the world. Hodcroft participates in the development of the open-source Nextstrain computer program, which tracks the evolution of pathogens.

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative











Join the conversation!