Could an ultrasound bath squeeze out mammograms?
Although mammograms remain the leading tool for breast cancer screening, doctors in Switzerland are exploring other ways of finding tumours at an early stage. An ultrasound bath that may be able to do the job without radiation or compression is one of them.
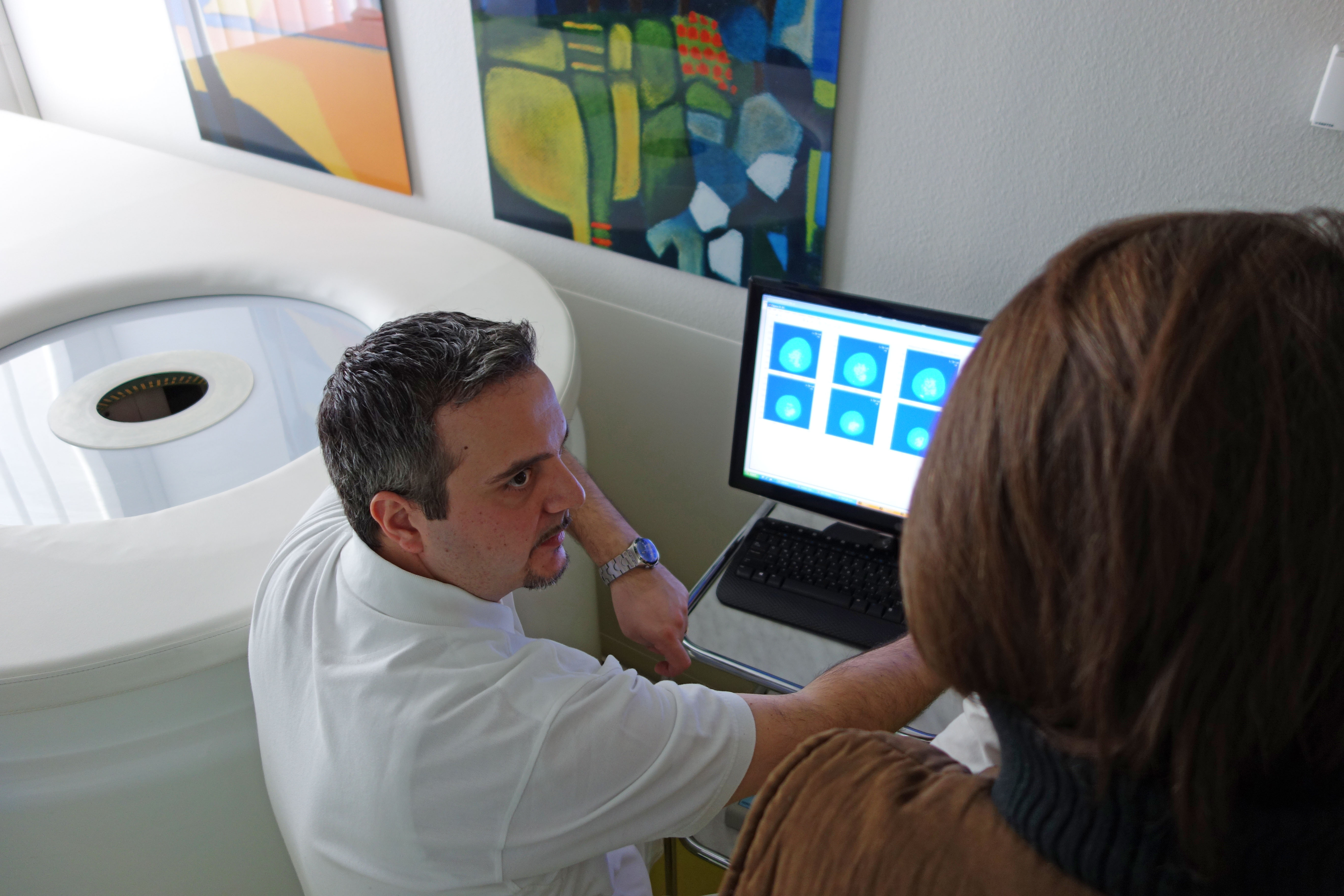
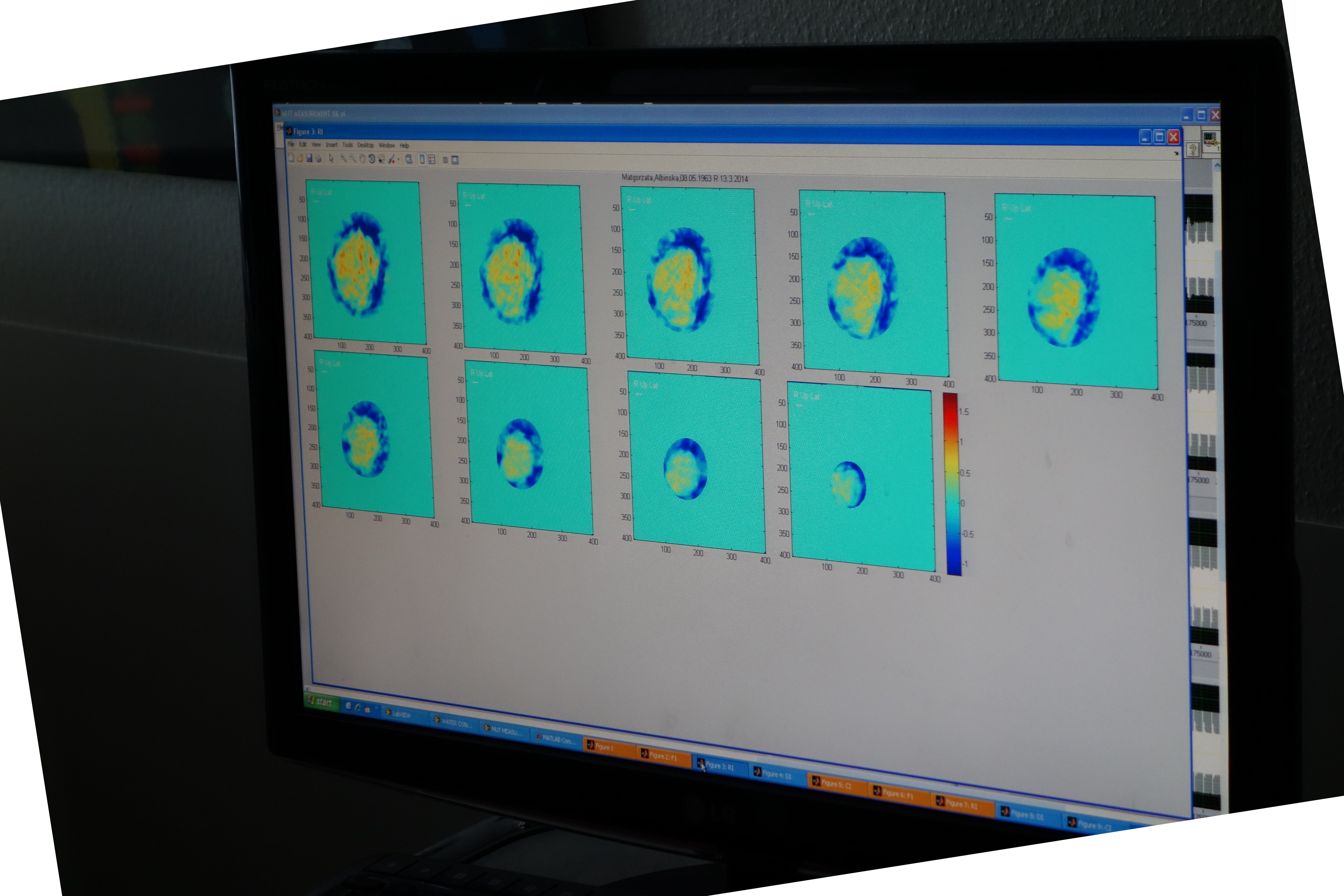
“You can do what you like, just don’t pull your breast out of the water,” as Serafino Forte tells his patient at Basel University Hospital’s breast centre. She’s lying belly down on a table with a round hole cut into it; her right breast is hanging into the basin below. Under the surface, ultrasonic sensors circle the tissue and send signals to a computer.
The patient, a 50-year-old who recently had her first routine mammogram, jokes that this is almost like a spa treatment in comparison. Mammograms can be painful as the breast is pressed tightly between the panels that capture the X-ray image. The tighter the squeeze, the sharper the images.
“After the mammogram I thought, ‘My God, isn’t there a method that’s a bit more comfortable?’ Then I saw a notice for this study, and I was curious,” she told swissinfo.ch. “This is much more comfortable. It all takes place in a fairly relaxed position, and you don’t really feel anything except for the water – kind of like when you’re in a bathtub and you move your hand underwater.”
Nor is there any radiation. A drawback is that it’s slow; it takes nine minutes to scan each breast, whereas mammograms are considerably quicker.
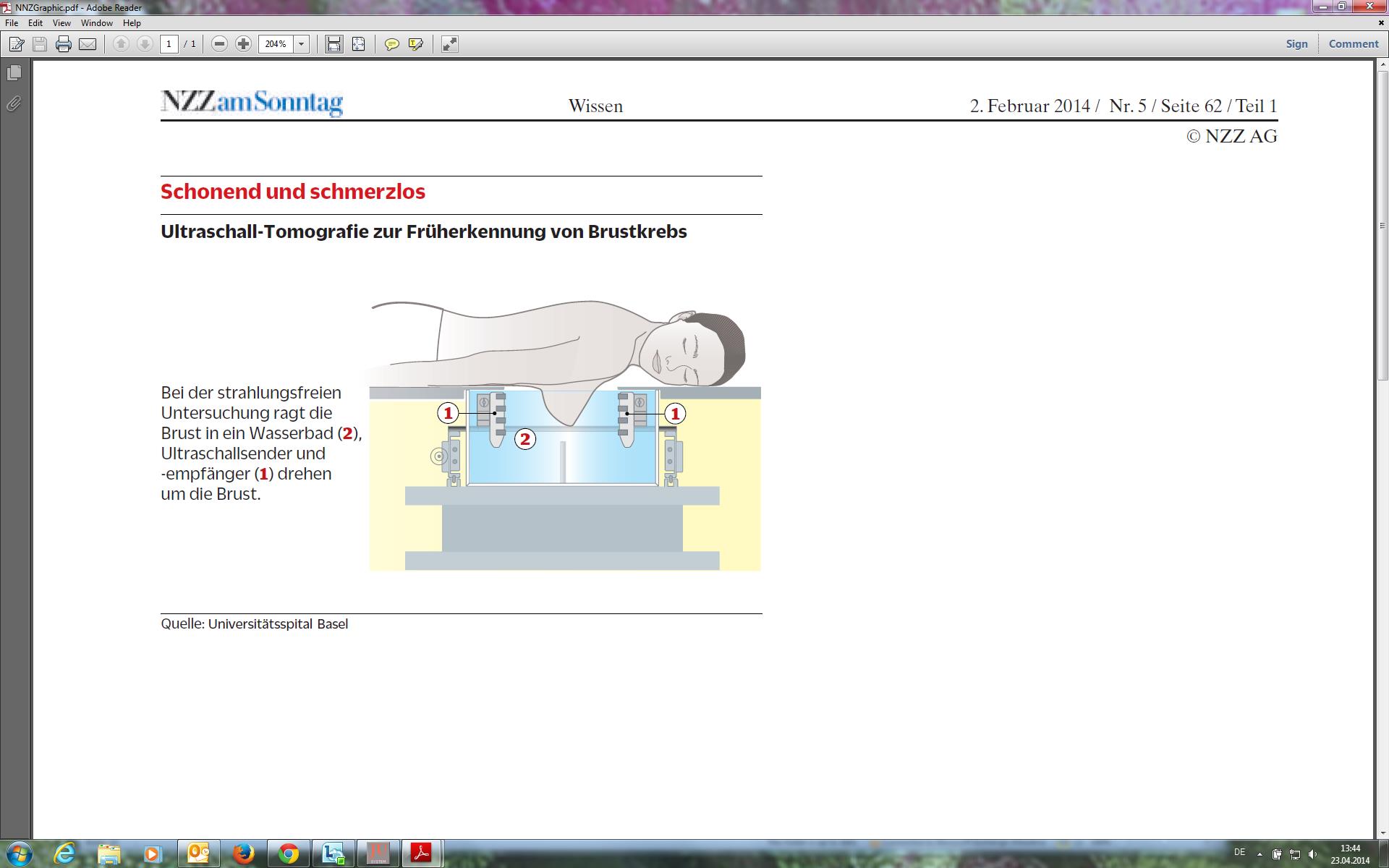
The technology is called “multimodal ultrasonic tomography” (MUT), and the prototype in Basel is the only one in the world. The idea came from Vasilis Marmarelis, a biomedical engineering professor at the University of Southern California; he was inspired by his wife’s experiences.
So far, the doctors in Basel have used the MUT prototype to scan more than 50 women; the goal is to examine 280 for the study’s first result. The only requirement is that the woman has had a very recent mammogram or other medical image for comparison. As it is still in the testing phase, it is not known whether it will produce the same level of data as a classic mammogram.
“All of the patients I’ve scanned so far have felt really comfortable. Some of the higher-risk patients have signed up for a follow-up in a year,” Forte told swissinfo.ch.
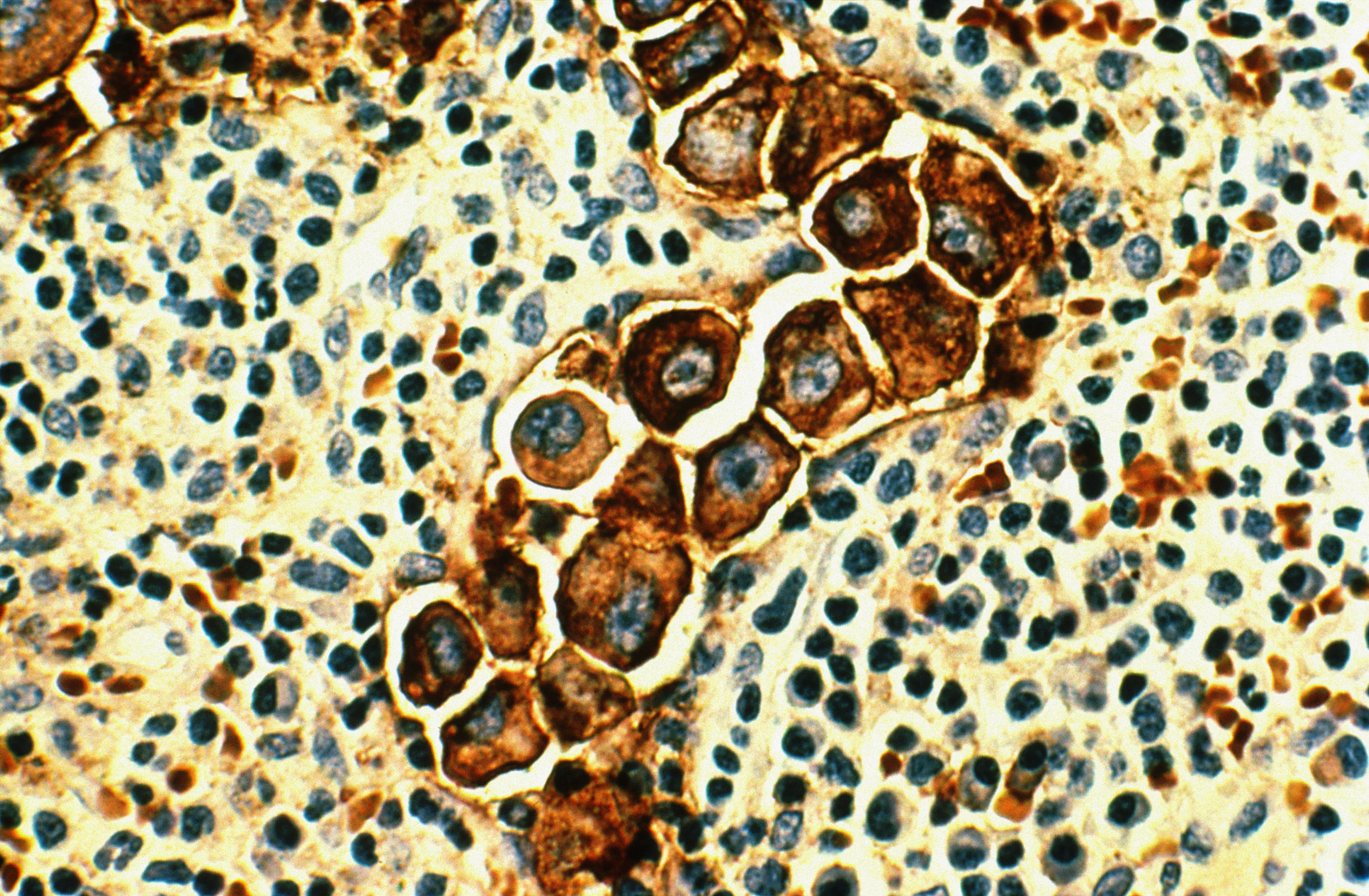
Some 5,400 women in Switzerland are diagnosed with breast cancer every year; another 1,400 die of it each year.
In June 2013, a national strategy was adopted to introduce widespread, quality-controlled mammography screening. Debate has since grown about the effectiveness of screening (see infobox), indirectly breathing new life into the search for alternatives.
Another promising technology is tomosynthesis, also an X-ray-based technique, but more sophisticated than mammography. Done regularly in Norway and approved by the US Food and Drug Administration, it’s also available in Basel.
“The very best, in my opinion, is tomosynthesis. This is the development for the future,” believes Sophie Dellas, the head of breast diagnostics at Basel University Hospital. The technology captures images of millimetre-thin slices of breast tissue, which are then converted via algorithm into more conventional-looking mammogram-style images.
“It can be done quickly and you have better sensitivity as well as specificity,” said Dellas, referring to a Norwegian study involving 10,000 women – also with dense breasts, which are more difficult to screen.
“There were fewer false positives,” Dellas said, in other words, fewer benign findings like cysts or fibre masses.
“The only problem with tomosynthesis is that it takes more reading time [than mammography],” Dellas said. And like mammography, tomosynthesis requires radiation and compression – a disadvantage in comparison to the MUT ultrasound bath.
Julia* was 61 when she went for a routine mammogram in Zurich in 2010 – something she’d been doing for a decade already. But this time, the radiologists saw something suspicious.
“The mammogram was not very clear. There was no discernible tumour, just calcification,” said Julia, whose gynaecologist referred her to the breast cancer practice in Seefeld for two biopsies. There she also had an MRI, and the doctors concluded that she would need a mastectomy.
“I wouldn’t have found out unless I had had the mammogram. From diagnosis to treatment, the whole process took only a matter of weeks. I was very happy with all of the medical advice and treatment that I received. The Swiss health service is wonderful,” the British woman told swissinfo.ch.
Julia’s case helps illustrate the importance of regular screening, and groups like the Swiss Cancer League and World Health Organization say that mammography remains the best bet for early detection of breast cancer.
Julia* – last name withheld
‘Not ready’
However, the MUT still has to prove itself.
“It would take a lot of work to show that it’s as good as or better than a mammogram,” Dellas said, highlighting the need for a B-mode version that would feature two kinds of ultrasound waves: ones that are reflected by the breast tissue, and ones that go through it.
“That would be real 3D,” Dellas said.
Mastoscopia, the Greek company that made the MUT prototype, is currently working on a B-mode module that should be ready this summer. When that happens, the study will continue as planned.
In the meantime, it seems mammography will remain the primary screening tool.
“It would be good to have an alternative, as we’re trying now. But we’re not ready to do screening with something else,” Dellas said.
In many parts of Switzerland today, women between 50 and 70 are encouraged to have a mammogram every two years. In June 2013, a national strategy was adopted to introduce widespread, quality-controlled mammography screening.
But in February 2014, the Swiss Medical Board (SMB) called for fewer mammograms – arguing that systematic screening has more cons than pros, and that it only saves one or two women out of 1,000.
“The mortality rate from breast cancer can be reduced slightly by means of the screening…[but] this desirable effect is offset by the undesirable effects. Specifically, erroneous results are produced in about 100 of 1,000 women with screening,” stated the board, which also described the costs-effectiveness ratio as “unfavourable”.
The board’s recommendation drew criticism from the Swiss Cancer League and specialists like Sophie Dellas, the head of breast diagnostics at Basel University Hospital. As she told swissinfo.ch, proper analysis of statistics is a challenge.
“If you’re analysing how many lives will be saved, only one in 1,000 is a lot if you have a country like the US or Germany, but it’s very few if you’re discussing a country like Switzerland. Also, you have to consider the loss of ‘life years’, and this is something that the SMB report doesn’t talk about,” Dellas said – referring to the number of healthy years a patient is able to enjoy.
False positives – and the resulting expense and worry that they cause – were another criticism of the SMB report. But according to Dellas, false positives – which could be benign findings like cysts or fibre masses – are simply a fact of screening.

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative










You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.