Malaria vaccine appears to be within reach
After 40 years of research and clinical testing, one of the great challenges of medicine looks as if it may be on the way to a solution: an anti-malaria vaccine, RTS,S, is currently undergoing clinical trials and showing promising results.
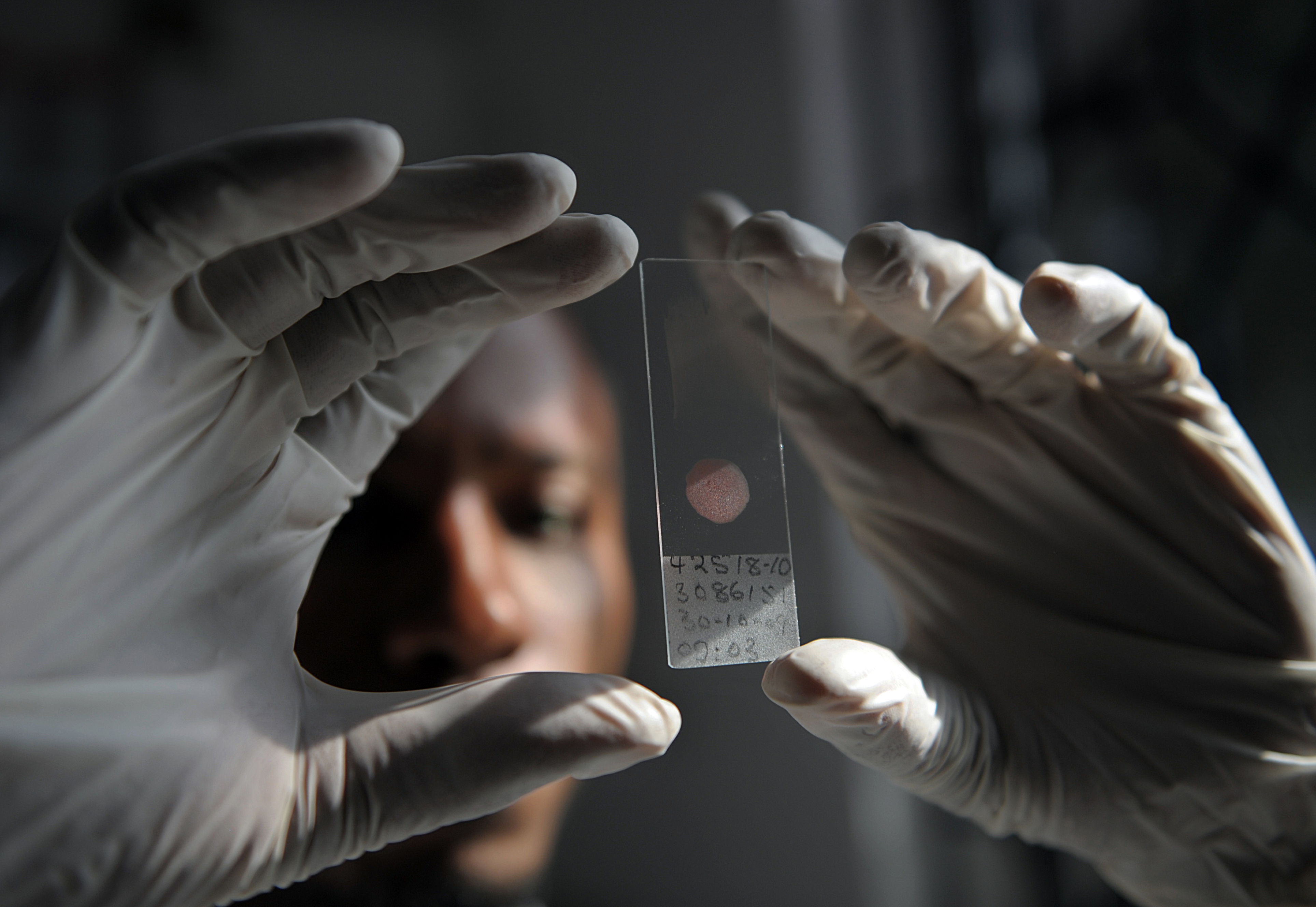
No-one claims that the battle against the disease – which kills about one million people a year – has been won. But of the 20 or so vaccines under development, testing of RTS,S is at the most advanced stage. Some 16,000 children aged between five and 17 months are taking part in phase III clinical tests in seven African countries. Initial results indicate that it halves a child’s likelihood of falling ill with malaria.
Knowing that most anti-viral vaccines are nearly 90 per cent effective, the figure might seem disappointing. But malaria is caused not by a virus, but by a parasite. Parasites change their skin much faster than virus and bacteria do; the anti-malaria vaccine will be the first to offer protection against any parasitic disease.
“It’s a matter of seeing the glass as half full or half empty,” says Blaise Genton, project leader at the Swiss Tropical and Public Health Institute in Basel, who has spent more than 20 years working on malaria vaccines, and is involved in the field tests of RTS,S.
“When you are working in malaria, if you halve the problem, you feel you’ve gone a long way. True, 50 per cent isn’t huge, but it’s much better than zero per cent. Admittedly, even this figure is theoretical, because we know we are never going to manage to vaccinate 100 per cent of children and achieve 50 per cent protection.”
“The important thing is that we have shown for the first time that a vaccine can work. This is a fundamental scientific breakthrough,” says Bernard Pécoul, Geneva-based executive director of the Drugs for Neglected Diseases initiative (DNDi).
“But if you are thinking in terms of public health, the figure of 50 per cent every 12 months – in other words, you need a booster every year – is not good enough for use on a wide scale.”
Despite these reservations, Genton and Pécoul agree that the vaccine represents an important victory in the fight against malaria. There is still a long way to go, but it is a major first step towards another vaccine, or a modified vaccine, which will be more effective.
Three approaches
The parasite is tenacious. It probably first infected human beings when they started to live in settled communities more than 10,000 years ago. The most dangerous form of the micro-organism responsible for malaria, plasmodium falciparum, learned long ago how to deceive its host’s immune system.
But once it has taken up residence inside the body, the parasite needs help before it can move on to its next victim. This is where the female anopheles mosquito comes in: she ingests the parasite when she takes a blood meal from an infected person.
After passing through various stages of its life cycle within her body over a period of about ten days, it is ready to be passed on to the next human being she bites.
There are three fronts on which the disease can be fought. One is to eliminate the mosquitos, or to stop them biting (for example through the use of mosquito nets permeated with insecticide); the second is to treat everyone who has been infected, to prevent the parasite from being passed on; and the third is to vaccinate those who have not yet been infected.
So the vaccine is not a panacea, but rather an addition to the current strategies for ridding the world of malaria.
Cost price
It remains to be seen whether the vaccine will be accessible to those who need it – some of the poorest people in the world.
Genton is quite optimistic. RTS,S was developed by the British company GlaxoSmithKline (GSK), which received massive support from the Bill and Melinda Gates Foundation, which is very active in the area of malaria: it has also put hundreds of millions of dollars into research carried out by the Medicines for Malaria Venture foundation.
“GSK will certainly not have a completely free hand in fixing a price,” Genton believes. “The price question is at the centre of discussion from the outset when these philanthropic initiatives are involved, and the funders have always said that the vaccine must not cost more than ten dollars a dose. It’ll probably even be a little bit less.”
So GSK is likely to follow the example of Novartis and the other major pharmaceutical companies working on malaria. Indeed, it has already said it will sell the vaccine at cost price.
No resting on laurels
Does that mean we might soon be seeing a malaria-free world? Genton, who is 12 years off retirement, dares not dream of such a thing in his lifetime.
He does, however, expect to see malaria eliminated in a number of countries where it is not very prevalent, but warns that there is likely to be “a slight increase in some countries where there are major conflict zones”.
He is also concerned that one of the knock-on effects of the financial crisis could be that states reduce their development aid and thus their involvement in the overall fight against malaria.
“But in the world as a whole there has been a decrease of nearly 50 per cent in some 20 countries. That’s a lot, and it shows that it’s possible to reduce malaria if we are give ourselves the means to do so,” says Genton.
“But it’s important that the governments of these countries should continue to regard malaria as a public health issue, even if the number of cases is falling. Because the moment you slacken your efforts, it will come back. We’ve seen this in Madagascar and many other countries.”
More than one million people die of malaria every year; in the world as a whole, 85% of malaria deaths are of pre-school children.
Africa accounts for more than 90% of all cases.
Malaria accounts for 40% national health budgets in African countries.
It costs sub-Saharan Africa $12 billion (SFr11.7 billion) in lost gross domestic product each year.
(Source: MMV)
A study published in May 2012 in the The Lancet Infectious Disease by researchers at the United States National Institutes of Health, based on 27 surveys carried out between 1999 and 2010 in seven countries in South East Asia and 21 in Africa, covering tests of 6,369 samples, revealed the following:
35% of anti-malarial medicines were sub-standard, containing either too little of the active principle, or an active principle that has since been banned because of its side effects.
46% in South East Asia and
36% in Africa were badly packaged or beyond their use-by date.
36% in South East Asia and
20% in Africa were counterfeit, where the active principle was either wrong or non-existent.
The authors of the study put the blame largely on China and India, the two main suppliers of developing countries.
They also point to the inability of local authorities to check the medicines they receive. For example, only three out of the 47 African countries where malaria is endemic, have laboratories able to conduct reliable quality control.
(Source: AFP)
(Translated from French by Julia Slater)

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative











You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.