
Swiss technology battles fake drugs
Counterfeit drugs have become one of the main health problems in developing countries. A device developed by three Swiss universities that identifies fake drugs could save the lives of hundreds of thousands of people worldwide.
“The phenomenon of fake drugs reached catastrophic dimensions a long time ago for the inhabitants of the world’s poorest regions,” said Claude Rohrbasser, retired head of industrial technology at the College of Engineering and Architecture of Fribourg.
“So several years ago we said to ourselves that with our knowledge and technological possibilities, we could do something to help these people.”
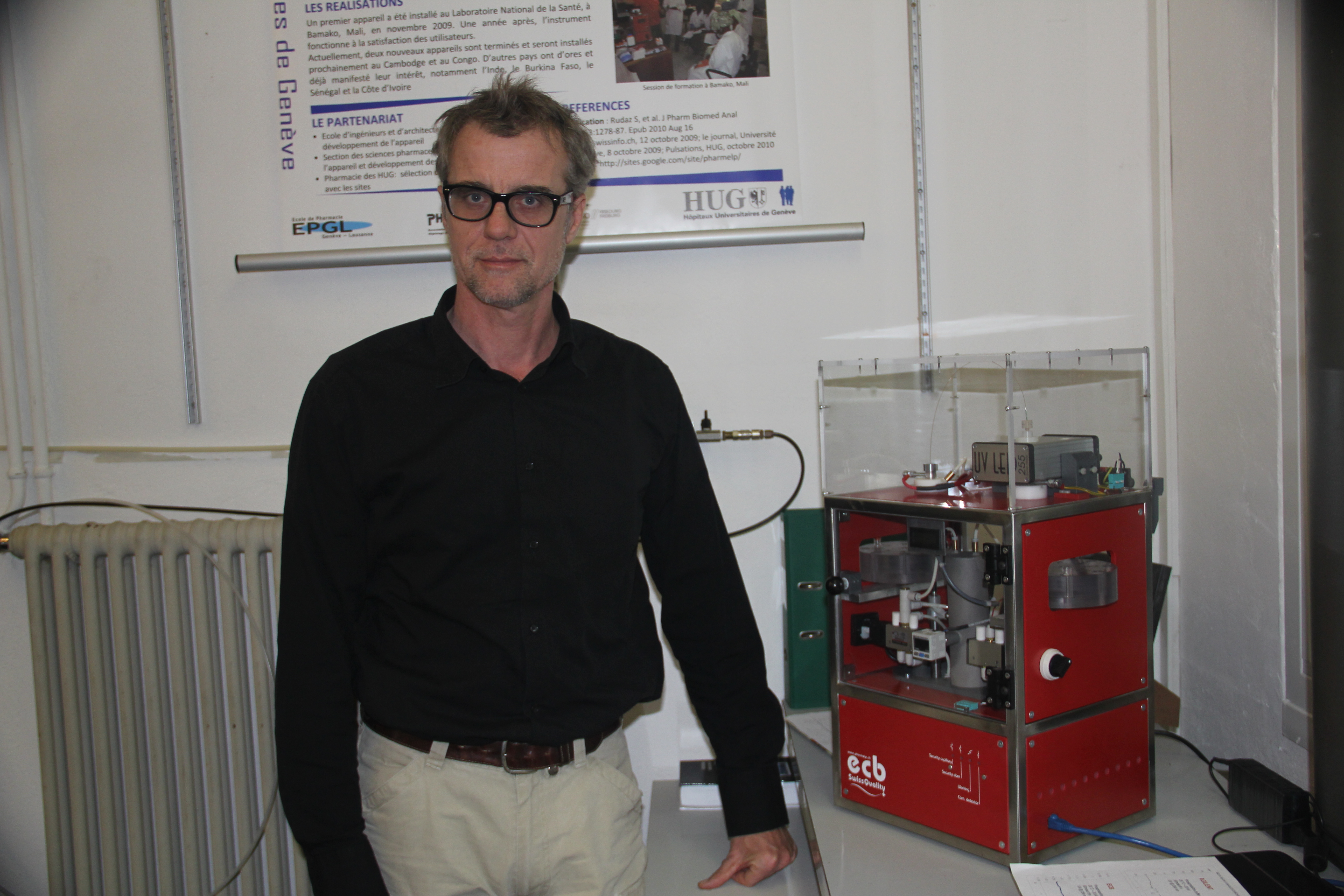
The Fribourg institute joined forces with the Geneva University Hospitals and Geneva-Lausanne School of Pharmacy to develop a low-cost system that identifies whether a drug is real or fake in just a few minutes.
The prototype of the ECB (budget capillary electrophoresis) was unveiled in 2008.
“The devices on the market cost at least SFr100,000 ($110,000). The ECB is only SFr10,000. For this amount we can find sponsors, whereas for SFr100,000 it would be pretty tricky,” said Rohrbasser, now president of Pharmelp, an association created by the initiative’s promoters to make the ECB available in developing countries.
Simple and effective
Despite its complicated name, the ECB represents probably the easiest – and at the same time most efficient – solution yet developed to detect and measure organic compounds, as well as drugs, proteins and amino acids.
The ECB enables the analysis of 80 per cent of the 200 core medicines identified by the World Health Organization (WHO).
“Our aim was to develop an instrument that was extremely robust and as simple as possible from a functional point of view. This was to reduce the problem of a lack of spare parts and facilitate the training of staff in the countries where it would be used,” said Serge Rudaz, associate professor at Geneva University’s School of Pharmaceutical Sciences.
Another advantage of the ECB is that it uses a minimum dose of solvent – barely a millionth of a litre – per analysis.
“In recent years, some solvents necessary for this analysis have gone off the market or have undergone major price increases, to the point of becoming unaffordable for health operators in developing countries,” Rudaz said.
According to the World Health Organization (WHO), less than 20 per cent of counterfeited medicines are comparable to the original product.
In more than 80 per cent of cases the counterfeited medicines do not correspond to the information in the package inserts, which can severely endanger patients’ health.
Thirty-two per cent of seriously altered mediciations don’t contain any of the active ingredient the medicine is supposed to contain, in 21 per cent the active ingredient differs from the original substance, in 20 per cent there is too little of the active ingredient, and in 8 per cent there are impurities in the drug.
Electrical pulse
The analysis takes just 20 minutes on average. First of all the drug is solubilised with water. A small quantity of the substance is set in motion by an electrical pulse (hence the name electrophoresis), then moves along a tube thinner than a hair (hence capillary).
Using ultraviolet rays, the device measures the duration of the drug’s journey, which is recorded on a normal laptop computer.
“The ECB can’t identify the medicinal composition – it verifies whether this duration corresponds to that of the original product. Each drug has its own charge and thus moves at a different speed,” Rudaz explained.
To date, the institutes have produced around ten ECB devices. The first three are already being used by the national health laboratory in Bamako, Mali, by Dakar University in Senegal and by the health authorities in Phnom Penh, Cambodia.
Other projects are planned in Congo, Ghana and the Ivory Coast.
Kidney problems
In these countries, a high percentage of drugs in circulation are counterfeit. In the majority of cases they are completely or partially lacking in the active ingredient listed in the packaging.
According to the WHO, these fake drugs are responsible for the deaths of hundreds of thousands of people a year around the world, including 200,000 people with malaria.
What’s more, for several years increasing numbers of impure drugs have been circulating, coming mostly from Asia.
“Over the long term, these attack the kidneys – we’re noticing more and more patients in poor countries who need dialysis. The consequences are terrible, given the meagre means available,” Rohrbasser said.
“Two years ago I visited the dialysis centre of the hospital in Bamako. There were ten or so patients lined up on beds. The head doctor told me they would die within a week because there weren’t any more filters for dialysis. This is another aspect of the problem of fake drugs.”
Official challenges
The trafficking of these drugs is tied to the inadequacy of health networks in poorer countries, above all outside the main inhabited centres. Many people get the drugs from travelling salesmen, who move from village to village.
“You’ve also got to bear in mind the tight financial circumstances. In many African countries people will normally buy only one or two pills at a time. And often they’ll do this at market, where prices are lower than in pharmacies and hospitals,” Rohrbasser said.
But the official sales channels aren’t without problems either. Political instability and war – as is the case currently in Mali – often obstruct the already precarious control measures for the drugs.
“But our aim is not to do the job of the police or customs – rather it’s to make available to the authorities, to hospitals and to universities an instrument which can identify fake products,” he said.
This pragmatism is shared by Serge Rudaz. “There’s no way we can solve the problem of counterfeiting in the countries with which we’re working. But our presence bears witness to the interest of our universities and of Switzerland in tackling the serious problems [these countries] face.”
Ten per cent of medicines distributed worldwide are counterfeited, says the World Health Organization (WHO).
In developing countries the percentage of counterfeited is medicines is as high as 30 per cent, whereas in industrialised countries the total is estimated at just 1 per cent.
Annual revenues from sales of illegal pharmaceuticals are estimated at around $75 billion. Between 2005 and 2010 the amount increased by 90 per cent.
WHO estimates that 200,000 people die from malaria annually because they are treated with counterfeited drugs.
Globally, it’s estimated that between 500,000 and 1 milllion people die annually as a result of counterfeited medications.
(Translated from Italian by Thomas Stephens)

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative















![The four-metre-long painting "Sonntag der Bergbauern" [Sunday of the Mountain Farmers, 1923-24/26] had to be removed by a crane from the German Chancellery in Berlin for the exhibition in Bern.](https://www.swissinfo.ch/content/wp-content/uploads/sites/13/2025/12/01_Pressebild_KirchnerxKirchner.jpg?ver=f05a5a9c)















You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.