Diabetes researcher proves the sceptics wrong

Zurich professor Marc Donath has developed a promising therapy, which targets the progression of the most common form of the disease.
He was the first Swiss to be awarded the Novartis Prize in Diabetes, the top honour in this field, at a recent congress in Rome. But, as he tells swissinfo, it has taken a while for his idea to be accepted.
Type 2 – which affects 90 per cent of diabetics and often occurs in later life – is on the rise, partly owing to unhealthy lifestyles. It affects up to seven per cent of the Swiss population.
It occurs because of problems with insulin, the hormone which controls glucose levels in the body. Type 2 diabetes patients cannot produce enough insulin or use it effectively.
Eventually the insulin-producing beta cells start to fail. Donath, professor of endocrinology and diabetes at Zurich University Hospital, identified the substance causing the cells to die and blocked it.
The blocker has been successfully trialled on humans using a drug normally prescribed for arthritis. The move, which has great industry interest, offers hope that diabetes sufferers may be freed from daily injections.
swissinfo: What is life like for someone with type 2 diabetes?
Marc Donath: At the beginning patients can reduce their need for insulin through lifestyle changes but as the beta cells progressively fail, they start needing tablets and eventually insulin injections. It’s important to realise that it’s a progressive and chronic disease, so you can delay it, but it’s ongoing and eventually, after ten to 20 years, you will need to replace your body’s insulin.
This typically requires multiple injections of insulin and when you inject, you have to know your blood sugar levels, which means measuring them several times a day.
swissinfo: How has your research made progress in tackling the disease?
M.D.: We started by understanding why these cells die and we identified the factor behind this. It is called interleukin-1 beta and is actually produced by the cells themselves.
Based on this we used a blocker of the interleukin-1 beta, which we tested in humans, the results of which we published in 2007. We showed that blocking can change something in the disease. Patients improved their blood glucose and more importantly they also produced more insulin.
This year we used a long acting blocker. We showed that it is safe and that it was sufficient to give one injection and still have a strong improvement in blood glucose over more than one month, meaning the patient can inject just once a month.
We were also impressed to see that after one month patients’ insulin production increased by 26 per cent and after three months this continued with 52 per cent more insulin production.
This is not a symptomatic therapy, just tackling blood glucose, but we really impact the disease’s progression. In fact, we could reverse the progression by increasing insulin production.
swissinfo: This would be a major breakthrough for sufferers to only need one injection a month?
M.D.: We are really working on this with several companies to make it available as quickly as possible. It is much more convenient for patients, especially because they have to take so many tablets and do so many injections that they sometimes forget.
It will probably take around three years for the first product to come on the market and other products may come a little later, in five to seven years.
swissinfo: There was a lot of scepticism when you first presented your idea.
M.D.: This is something that often happens in science when you change a paradigm. What we have described is a specific type of inflammation. People didn’t believe that this inflammation had anything to do with type 2 diabetes and there was quite strong scepticism, especially within the European community.
So it was quite rewarding to feel at the international diabetes meeting in Rome that the concept is now really accepted. Importantly for us, several groups have now independently confirmed our findings and this is what in science at the end of the day convinces people.
swissinfo: So it has been a difficult path?
M.D.: It was definitely a difficult path on several levels: personally, because if people doubt you, you start to doubt yourself and if a cloud of doubt is hanging over you, then it is more difficult to publish your data and find money for your research.
The first turning point was in 2007 when the first group confirmed our findings and we published in the renowned New England Journal of Medicine. The second turning point came after we confirmed everything with a second trial this year. Now people start to say it was obvious all along and the enemy from before now wants to be your best friend – but this is typical of human beings.
It was nice to receive the Novartis prize, as the selection committee is made up of people I have a lot of respect for – the top names in diabetes research. It was another recognition.
swissinfo: How will you go about testing for safety?
M.D.: First we have to find out the perfect dose and how long we will have to administer the drug… Then we go to phase three trials, lengthy safety trials. Safety is the issue for any drug, but especially in diabetes because a few other drugs turned out to have safety issues.
I’m optimistic because a similar treatment is already given to patients with rheumatoid arthritis and it looks very safe. Because we understand quite well the biology of what we are doing I don’t think there will be side effects.
In the pessimistic event that the drug does not make it because of side effects, we have described a pathway. So even if this drug didn’t work we can still imagine having another drug working on the same pathway. So overall I’m optimistic we’ll get a drug based on this finding.
swissinfo-interview: Isobel Leybold-Johnson in Zurich
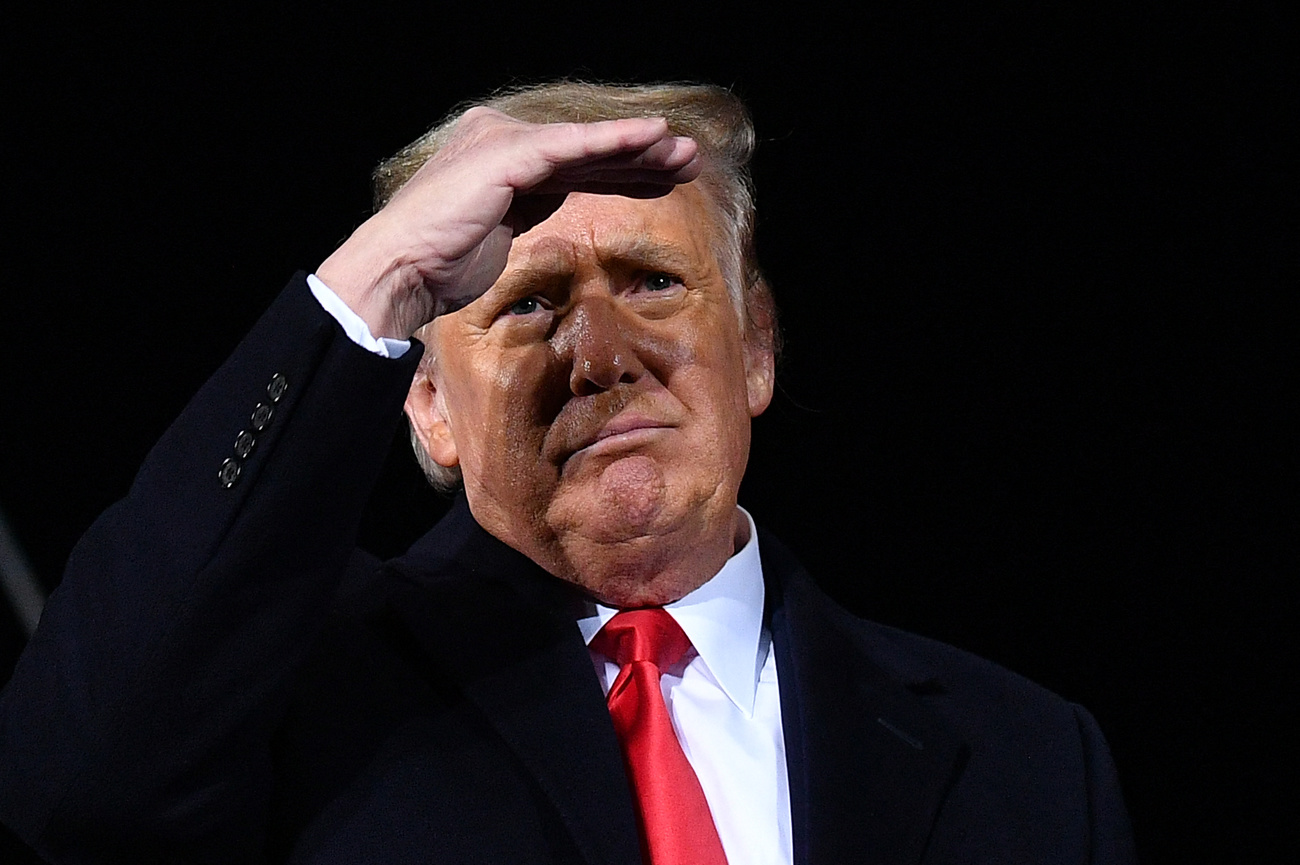
Donath, 44 years old, is a professor of endocrinology and diabetes at Zurich University Hospital.
He comes from Geneva, but has spent most of his career in Zurich, with a two-year stint in Jerusalem.
He is a practising doctor with patients and divides his long working weeks between his research, patients and administrative duties.
He received the $25,000 (SFr27,600) Novartis Prize in Diabetes on September 9 at the European Association for the Study of Diabetes meeting in Rome.
Many patients who develop the disease are overweight and most are in the 40-59 age band, but children and young people are becoming increasingly affected. Once developed the condition persists throughout a patient’s lifetime.
Around 6-7% of the population have the disease in Switzerland. In the United States, it is around 10%. Genetics can also contribute, and poor countries that suddenly adopt a high calorie diet have been found to quickly develop the disease. In some areas this can be as high as 50 per cent of the population.
In the next 20 years the number of those affected is expected to rise to 380 million worldwide, reaching epidemic levels.
Type 1 diabetes is where the body attacks its own insulin cells. This is prevalent in children and these young patients need burdensome insulin injections. Donath is hoping he can apply his knowledge of type 2 mechanisms to develop a therapy for type 1. Trials could start next year.

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative










You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.