Hospitals feel the ‘Angelina Jolie effect’

Swiss hospitals have seen a leap in women choosing to test for a breast and ovarian cancer gene in what has been dubbed the “Angelina Jolie effect”. But in contrast to the United States, in Switzerland there is less of a move to follow the actress’ lead and have preventative surgery once the gene is found.
Jolie went publicExternal link about her double mastectomy in 2013, undertaken after discovering she had the faulty BRCA1 gene, placing her at an increased risk of developing breast and ovarian cancer. In March 2015 she revealed that she had had her ovaries and fallopian tubes removedExternal link. Her mother had died of ovarian cancer at the age of 56.
The publicity around Jolie’s mastectomy has led to an increase in women around the worldExternal link External linkasking for BRCA gene testing. The gene BRCA 2 also carries an increased cancer risk.
“We have 30-40% more genetic counselling consultations since Angelina Jolie went public in 2013,” Dr Patrizia Sager, head of breast diseases at Inselspital, Bern University Hospital, told swissinfo.ch from her consulting room in the hospital’s breast centreExternal link.
Other hospitals in Switzerland, such as in GraubündenExternal link or LucerneExternal link have also reported the Angelina Jolie effect.

But while Sager welcomes the increased awareness, she also sounds a note of caution. “Only 5-8% of breast cancer patients have the gene mutation, so most breast cancers are not due to a gene that we know of now,” she said.
“Today a lot of people who have had one grandmother with breast cancer in the family history are afraid to have the gene. However, it’s very seldom that that you have it.”
Testing for genes
More than 50% of genetic consultations currently end up in a BRCA gene blood test. One of the laboratories to which they are sent is based at the Cantonal Hospital in AarauExternal link. It carries out the most BRCA gene tests in in German-speaking Switzerland.
DNA is extracted from the blood and the two BRCA genes are isolated, amplificated, and then tested for the mutation, he said.
Lab head, clinical geneticist Benno Röthlisberger, said test requests had more than doubled since 2013. “We have over 500 requests a year now,” he told swissinfo.ch.
Full genetic screening, when the gene is not known in the family, costs up to CHF4,000 ($4,162). If the mutation is established, testing additional relatives costs less than CHF400. Both are covered by the health insurance if the family history is striking enough.
If a BRCA mutation is found the risk of a woman developing breast cancer during her lifetime is 80%, Röthlisberger explained. In terms of ovarian cancer, for BRCA1 the risk is up to 50% and for BRCA2, up to 30%.
Two options
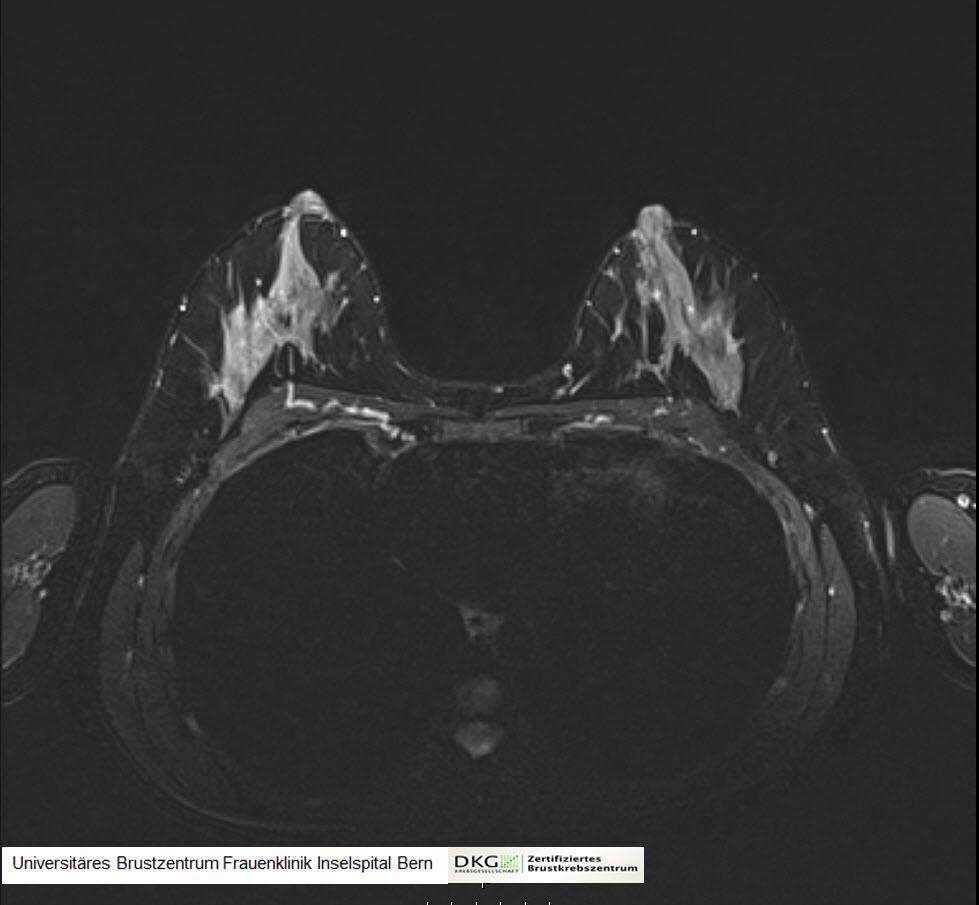
A woman faces two options if she is found to carry a BRCA gene. Either she can opt for monitoring, for example, a breast MRI every year and half yearly ultrasounds. Or she can have breast and/or ovarian removal, basically taking out healthy tissue to avoid an occurrence of cancer in the future. This option is recommended for women over 35 who have stopped childbearing.
Switzerland is not as radical as the United States, where, Sager says, doctors often recommend preventative mastectomy, rather than monitoring. Overall the US approach is more aggressive.
“If someone has breast cancer but not the gene, in Europe we try to conserve the breast and not remove everything. We know that the outcome is just as good,” Sager continued. “In the US it is more common to remove the whole tissue and make an implant or reconstruction.”
In patients with the BRCA gene, removing the breast tissue can reduce their risk of developing the disease to the same level as the rest of the population – 10% – or even a bit less, Sager said. Totally eliminating the risk is not possible.
Removing the ovaries is recommended because it is difficult to screen for ovarian cancer. It also reduces the risk of breast cancer.
Younger patients normally choose close monitoring, with possible surgery later.
Having an operation is, nevertheless, a difficult decision, Sager says, as it goes to right to core of a woman’s sense of being. Breasts will need reconstruction; the removal of the ovaries means an early menopause.
Although she can’t give exact figures, the number of breast removals has increased since 2013, Sager said. Awareness and acceptance of this as an option has risen, she noted.
Faulty genes
BRCA1 and BRCA2 are genes that produce tumour suppressor proteins. These proteins help repair damaged DNA and therefore play a role in ensuring the stability of the cell’s genetic material. Should either of these genes become mutated, such that its protein product is not made or does not function properly, DNA damage may not be repaired properly. So cells are more likely to develop additional genetic alterations that can lead to cancer.
Source: National Cancer Institute, United States
Tackling a taboo
Sandra Schallberger, 42, took the operative route earlier this year after finding out she carried the BRCA1 mutation. Her mother had died from ovarian cancer.
“I knew before I took the test [what I would do],” Schalleger, who had the surgery at Inselspital, told swissinfo.ch. “I knew just talking with my mum during her illness that if she had had the chance, she would have chosen to have her ovaries removed after having a family.”
“So after I was sure I did not want many more kids, I had both breasts and ovaries removed at the same time,” said Schallberger, speaking from her home just outside Bern, where the garden shows evidence of two small children. She describes them as her motivation for having the procedure.
It was, however, a big step, Schallberger says and she understands that not everyone is ready to do this. For her, however, a burden has been removed.
She took the gene test before Jolie’s announcement, but has seen another effect of the star’s decision to go public.
“It has made it easier for me to talk to other people about my operation,” she said. “People are now more understanding about why I chose this way.”
“When people didn’t know about the subject, it was hard for them to understand why you would remove something that isn’t ill, as a prophylaxis. Angelina Jolie has brought an awareness to people that there is such a thing as prophylactic surgery.”
Will the Angelina Jolie effect continue? Sager says it is hard to say for sure, but Jolie and other celebrities talking about breast cancer have certainly put the issue into the public sphere. “So probably it’s become more common for people to get informed,” she said. “You want to know: what is the risk for me?”
Breast and ovarian cancer: the statistics
In Switzerland, around 5,500 women develop breast cancer a year. It is the most common cancer among women, accounting for one third of cancer diagnosis among women. 80% of those affected are over 50 years old at diagnosis. 40 men develop the disease per year.
Ovarian cancer affects 600 women per year in Switzerland, accounting for around 3% of cancers in women. It mainly develops in later years, but 14% of patients at under 50 at the time of diagnosis.
Souce: Swiss Cancer League

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative









You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.