The delicate challenges of fighting Ebola

‘Sometimes I am embarrassed to talk about Ebola’. These were the words of World Health Organization Director General Dr Tedros Adhanom Ghebreyesus, opening a high-level meeting in Geneva this month on the Ebola outbreak in the Democratic Republic of Congo.
His point is a valid one: DRC is a country with many humanitarian and health challenges. As Dr Tedros pointed out, measles is among the biggest threats to DRC’s children, and has claimed far more lives in DRC than Ebola. In managing the very difficult Ebola operation, the WHO knows it must take care not to neglect other health challenges.
But two days after that meeting, the WHO declared DRC’s Ebola outbreak to be a public health emergency of international concern. The discovery of a case of Ebola in the city of Goma, population almost two million, and close to Rwanda’s border, plus growing pressure from health experts and aid agencies, meant the WHO had little choice.
Why the delay?
For months now, observers of this outbreak have warned the WHO that the conditions for declaring an emergency (what’s called a PHEIC in WHO jargon) have long been met. An international emergency does not require multiple case of Ebola in multiple countries, simply the risk of the disease spreading across borders is enough for a declaration.
“Until now, the WHO hasn’t called an emergency because it fears repercussions in the form of travel restrictions. But the status quo is no longer tenable,” said Professor Lawrence Gostin, a specialist in public health law at Georgetown University.
“We need a sense of international urgency, mobilizing resources, and deploying experienced personnel.”
More
Aid money: spending every penny wisely
Staying safe and building trust
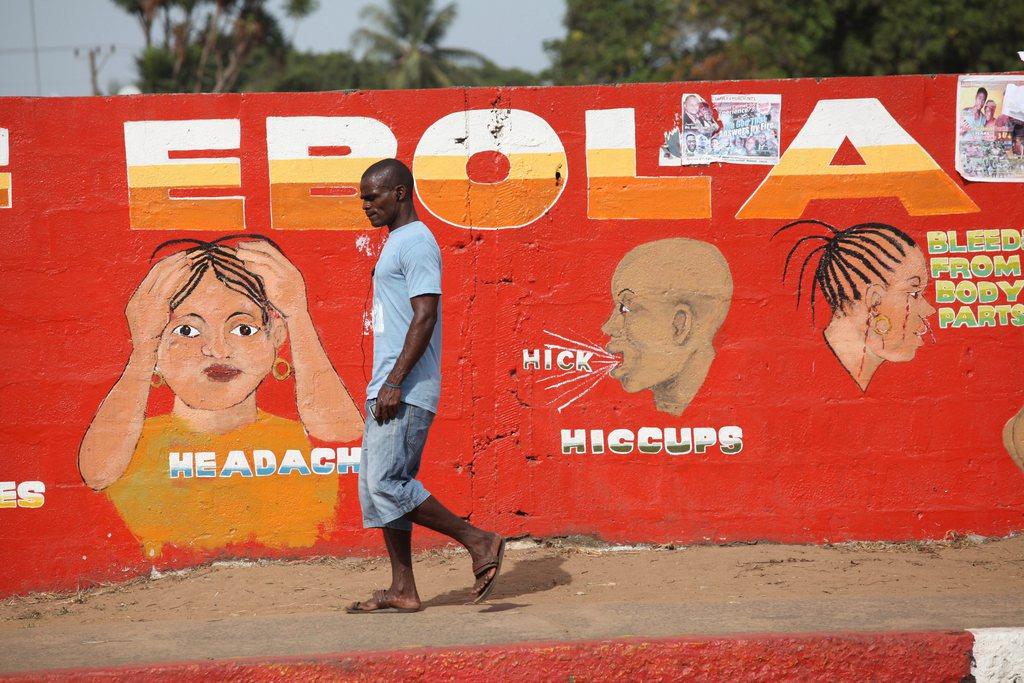
One of the key challenges in this Ebola outbreak, and the key reason new unrelated cases keep appearing, is safety. The disease is spreading in conflict areas, communities are suspicious of international aid agencies, some health responders have been attacked and killed.
In such a climate, tracking and treating everyone who may have come into contact with Ebola becomes impossible.
Professor Gostin suggests creating a ‘safety zone’ for health workers entering villages to treat Ebola patients, with United Nations peacekeepers alongside to protect them.
But aid agencies like Médecins sans Frontières and the International Rescue Committee, both of whom have been working in DRC since the start of the outbreak, see it differently. They want more community engagement to build trust, and the IRC added ‘a demilitarisation of the process.’
“The inability to build community trust has proven a major barrier to stopping the spread of this disease,” the IRC said in a statement. Local communities are perplexed and frustrated by a continued increase in the number of people dying juxtaposed with a massive influx of international organizations into the region during the past year.”
And Joanne Liu, president of MSF, added health workers needed to humanise the process of treating people with Ebola, and involve their families more closely in the process.
“Could we think of having a decentralised approach to treat patients, and not putting them somewhere with only spacemen around away from their loved ones?” she said.
Differing views
These differing views on how best to handle the outbreak reveal just how tricky it is. Scaling up the military response may simply fuel lack of trust, and could even act as a trigger to yet more violence.
But without at least some form of protection, health workers will be unable to reach all the Ebola-affected areas.
What’s more, there are quiet voices inside the heath agency who suggest that declaring the PHEIC simply won’t make any difference, other than to generate a few headlines, focus international attention for a short period, and, perhaps, generate some more funding.
Extra cash could be useful; at the moment DRC’s Ebola outbreak is dismally funded compared with the funds made available to West Africa five years ago.
But again, because of the insecurity, it is not clear exactly what extra money, if it ever arrives, would be spent on. After all, what is the point in new teams of health workers, if conflict stops them working safely, or of even getting to the places they need to work?
Vaccine transparency
Perhaps one important area for fresh investment is in vaccines. The one bright spot from the devastating outbreak in West Africa has been the development of a successful vaccine against Ebola.
In DRC today, health workers and those who have come into contact with Ebola patients are receiving the vaccine. Without it, this outbreak would already be far worse.
But MSF’s Joanne Liu, looking at the insecurity in DRC, and the challenges to trace those who could be infected, believes the vaccination campaign needs to be ramped up.
“We should have a geographical approach,” she explained. “Meaning that if someone is infected coming from (a) village, we would not only vaccinate the contacts and the contacts of contacts, we would vaccinate the whole village.”
A good plan perhaps, except that it is unclear if there are enough vaccines to actually do this. In fact, no one knows exactly how many doses of the Ebola vaccine exist.
“We are told it is between 250,000 to 500,000 doses,” said Liu. “So… where are they? When will they be available? We need much more transparency and clarity about the status of vaccine supply today.”
No shortage of ideas
And so, as it continues to try to get control of DRC’s Ebola outbreak, the WHO is not short of suggestions as to how it could do a better job.
Community outreach, trust-building, these are surely on the WHO’s to-do list. Calling the emergency should not, Dr Tedros insisted, be a reason to stigmatise or penalise the very people who need help.
And that is exactly why he mentioned measles, before declaring the Ebola emergency. The best way to build trust, in this complex and highly dangerous Ebola outbreak, may be for the WHO to continue with its regular health interventions. The ones the community is used to, the ones mothers know will save their children’s lives. And side by side with that, ask, listen, explain, and treat, Ebola.
You can follow Imogen Foulkes on twitter at @imogenfoulkes, and send her questions and suggestions for UN topics.

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative











You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.