‘Dealing with dementia sufferers needs time and patience’

Switzerland has an ageing population – which also means more dementia cases. A residential care home in Biel offers dementia patients a sense of security, while also allowing them a certain amount of freedom. swissinfo.ch went to have a look.
There are eight dementia sufferers – six women and two men – living in the three-storey house in Biel, a town not far from the Swiss capital, Bern. They are between 73 and 89 years old. Some are active and mobile, others are in need of constant care. They can all stay here until they die.
In the entrance hall we meet F.L*. The 83-year-old woman, who has been living in the care group for three months, is looking for her son. Have we seen him? No, we say. What’s his name? “Renzo, do you know him?”
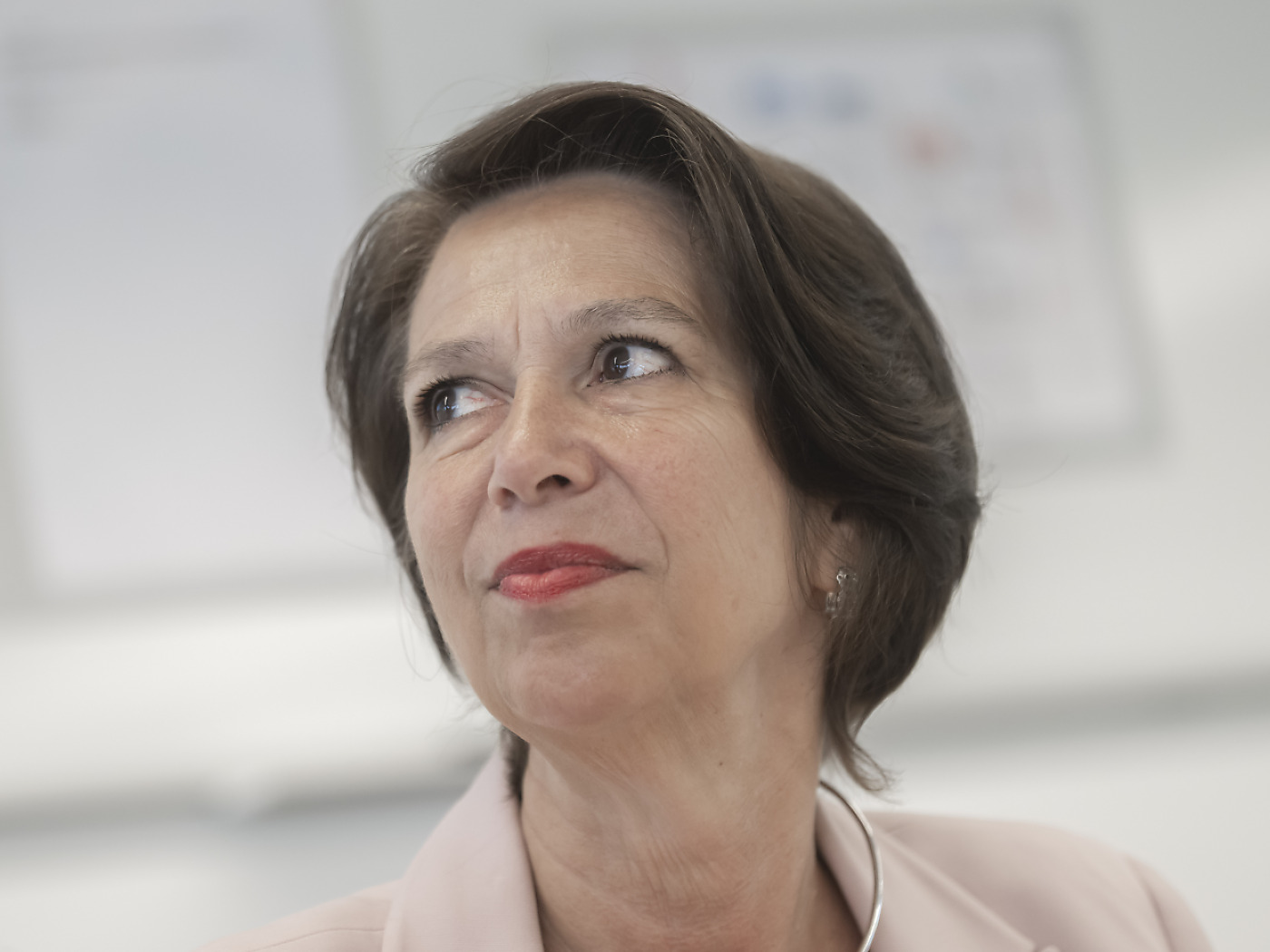
It’s typical for dementia sufferers to look for their children or even their parents, says Marianne Troxler-Felder, co-home and nursing manager at the Care for the Aged Association Biel-Seeland. “Dementia sufferers feel much younger than they are and often live in the past.”
The unfamiliar and the familiar
S.V.*, also 83 years old, seems confused, restless and a bit lost. Just 150 centimetres tall, and wearing a wool beret on her grey hair, she doesn’t know where she is or what she is doing there or where her husband is. “He was a horrible man when he was in a bad mood, but we had a good life.”
She spent 50 years in her flat, where everything was familiar. Now nothing is. “When are we going home? Where is my handbag?”
S.V. enjoys being in the garden. It’s not just a garden for her, but a place where she can busy herself with her chores, such as going to the bank and shopping. Today she is accompanied by nurse and care home manager Brigitt Rohrer.

More
A walk in the garden
The inconspicuous yellow house in Biel, which has been a care home for ten years, dates from the 1930s. It has seen better days – like many of its residents. But this is to its advantage, says Troxler-Felder.
“People feel a sense of security here. It’s small and manageable, just like being at home. This means that all types of stimuli, which dementia suffers find increasingly difficult to deal with over time, can be better reduced than in a larger institution. But some people find it too small. They need more space and so are better off in a larger establishment.”
In one of the two living rooms on the ground floor there is a tile stove, in the other, a television. “We don’t watch much television, because it’s too fast for most people. Sometimes we watch a bit of sport or a music programme, but one of us is always present,” Rohrer says.
Some residents like flicking through newspapers and magazines, as they used to do, concentrating on the headlines and the pictures. “But they can no longer remember what they have read,” Rohrer explains.
Dementia is an umbrella term for various brain disorders. It is defined by a memory disorder, combined with the loss of several other brain functions, such as speech or movement. Both lead to a loss of independence.
Alzheimer’s is the most well-known and common form of dementia.
The biggest factor in dementia is age, with the risk of developing the disease rising after the age of 65. 8% of the over-65s are estimated to be affected by Alzheimer’s and other forms of dementia.
There are more than 110,000 dementia sufferers in Switzerland. This number is predicted to rise to 200,000 by 2030 and to around 300,000 by 2050.
Worldwide there are around 44 million people suffering from dementia, 25% more than three years ago. This could rise to 76 million by 2030 and 135 million by 2050.
(Source: Federal Statistics Office, Swiss Alzheimer’s Association, Alzheimer’s Disease International)
Kitchen meeting point
The heart of the house is undoubtedly the kitchen: here people drink coffee together, eat and play games. Residents are encouraged to take part in daily life, such as helping to fold and iron the washing, peel the vegetables or empty the compost. Structure is important and gives the residents a secure footing. In addition, two ladies offer memory training, exercise or singing one afternoon a week.
A crucial factor is that the patients feel accepted and are not constantly corrected, says Rohrer. “We fetch them from where they are and try to, at best, bring them back into present life. Some of them realize in the meantime that there is something wrong with them but they can’t put their finger on it. This can result in fear and panic.”
Dementia patients need a lot of time and patience, Troxler-Felder says. “Do it fast, chop, chop! This doesn’t work at all.”
There are normally two to three caregivers in the house, plus an apprentice, and they know their charges very well. “We can tell with those who can’t speak from the colour of their faces, their body language or their gestures if they are unsettled or worried,” Rohrer explains. “It’s important to have a day-to-night rhythm, exercise and fresh air, she adds.
Freedom to move
Dementia sufferers are often restless and need to move about. But they mostly don’t have a sense of time or orientation. That’s why it’s better for them to live in a protected area. But the concept behind the dementia care home includes allowing them as much freedom of action as possible, even if this involves a few risks.

More
A tour of the house
Switzerland drew up a national dementia strategy at the end of 2013.
It is aimed at promoting a better understanding of dementia among the population and specialists. It wants to ensure that all people suffering from dementia have access to high-quality, low-threshold and continuous provision of integrated psychosocial, medical and nursing care, and that these patients and those closest to them have access to a full range of information. The authorities should provide more respite services for relatives and improve care in homes.
How this will be financed
is not yet clear. The Swiss Alzheimer’s Association has pointed to this being a sticking point.
The two upper floors, which can be reached with a stairlift, house the residents’ bedrooms. These are furnished with a bed and bedside table. Other furniture can be brought from home. On almost every bed sits a stuffed toy, and family photos are also popular. Some residents, like Madelaine Blank, have drawings by grand or great-grandchildren. The 80-year-old has been living in the Biel house for a year. There’s a picture by her great grandchild Sofie on the wall; on the table stands a framed photo of Mr and Mrs Blank.
Her husband, also 80, visits several times a week, and they always eat together on Thursdays. “They serve us the food in the room, with a tablecloth and flowers. We’re really spoiled,” René Blank says.
On Sunday he takes his wife home and cooks whatever she wants. “She wolfs down salad. I’m happy to do something nice for her and to bring her out of her usual daily routine.”
Madelaine Blank first showed signs of depression ten years ago. Then, around one and a half years ago, she refused to get up and stayed in bed for three months. The diagnosis: Alzeheimer’s. She also suffers from macular degeneration, which limits her eyesight. She can just about manage large letters with the aid of a reading device. She can no longer sew or knit like she used to do.
Looking after his wife on his own became too much for René Blank. He particularly found it hard that she no longer took part in daily life. “It was only after they doubled the psychotropic drugs, after three months, that things started to settle down.”
Much has changed in the couple’s life. “I’ve had to learn that separation doesn’t just happen with death, it can also happen through illness,” René Blank says.

More
How the Blanks cope
It’s now evening and the scent of warm apples and cinnamon permeates the house. People are sitting down to dinner in the kitchen – except F.L. She is still looking for her son, Renzo.
*Names withheld
(Translated from German by Isobel Leybold-Johnson)

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative








You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.